About Us
At ExquiroLogix RCM, we empower healthcare providers to focus on what matters most—delivering exceptional patient care. With our deep expertise in medical billing and credentialing, we navigate the complexities, streamline operations, and maximize efficiency, so you can dedicate your time where it’s needed most—your patients.
We specialize in serving individual providers, clinics, and hospitals. Our goal is to optimize your revenue cycle, streamline administrative workflows, and ensure your practice remains compliant with the latest regulatory changes, allowing you to focus on what matters most—caring for your patients.
Our mission is to provide exceptional service with an unwavering commitment to quality and customer satisfaction. Our 24/7 Contact Center Solutions ensure a seamless experience for your clients every day of the year. By prioritizing excellence, we not only enhance your brand’s reputation but also help reduce operational costs by 35-40%.






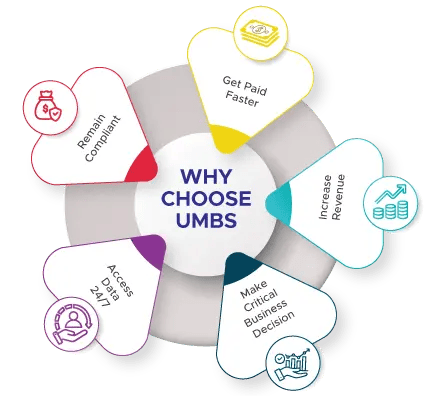
Why Choose US
Because we care about your success! We’re dedicated to providing you with personalized, efficient solutions that make your life easier. Our team is passionate about ensuring your practice runs smoothly, using the latest technology and offering clear communication every step of the way. With us, you’re not just another client – you’re a valued & trusted collaborator, and we’re here to help you thrive.
Our services
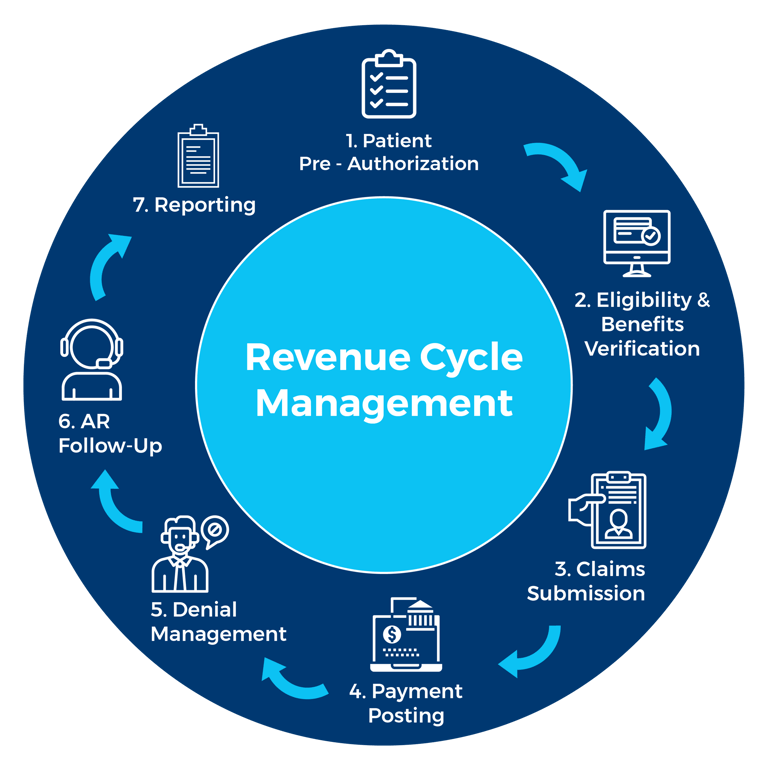
Revenue Cycle Management Computer Process
Patient scheduling ensures accurate documentation, timely billing, and smoother coordination with insurance, leading to faster payments and fewer errors.
Patient Scheduling
Patient scheduling is crucial for medical billing as it ensures accurate coding and timely documentation, leading to correct billing. It helps in:
Accurate Billing: Proper scheduling ensures the right services are documented, minimizing billing errors.
Efficient Revenue Cycle: Scheduled appointments improve claim submission, reducing delays and no-shows. Faster
Payments: Pre-scheduled appointments allow for insurance verification and necessary authorizations, speeding up the payment process.
Better Coordination with Insurance: Ensures pre-authorization and accurate patient data, reducing issues with insurers.
Patient Satisfaction: Clear scheduling helps avoid confusion, improving patient experiences and ensuring all services are billed properly.
In short, good scheduling streamlines the billing process, reduces errors, and ensures timely payments.
Patient Demographic
Accurate patient demographics ensure smooth medical billing, prevent claim denials, and support efficient healthcare operations.
Patient demographics are essential for accurate billing, preventing claim denials, and ensuring efficient healthcare operations.
Accurate Claims Processing – Correct details (name, DOB, insurance info) prevent claim rejections and delays.
Insurance Verification – Ensures eligibility and proper coordination of benefits.
Avoiding Denials – Errors in demographics are a leading cause of claim rejections.
Faster Reimbursements – Reduces administrative workload and improves revenue cycle management.
Effective Communication – Ensures smooth patient-provider interaction for follow-ups and billing.
Legal Compliance – Meets HIPAA and other regulatory requirements.
Medical Record Accuracy – Supports continuity of care and prevents patient mix-ups.
Maintaining up-to-date demographics enhances billing efficiency, patient experience, and revenue management.
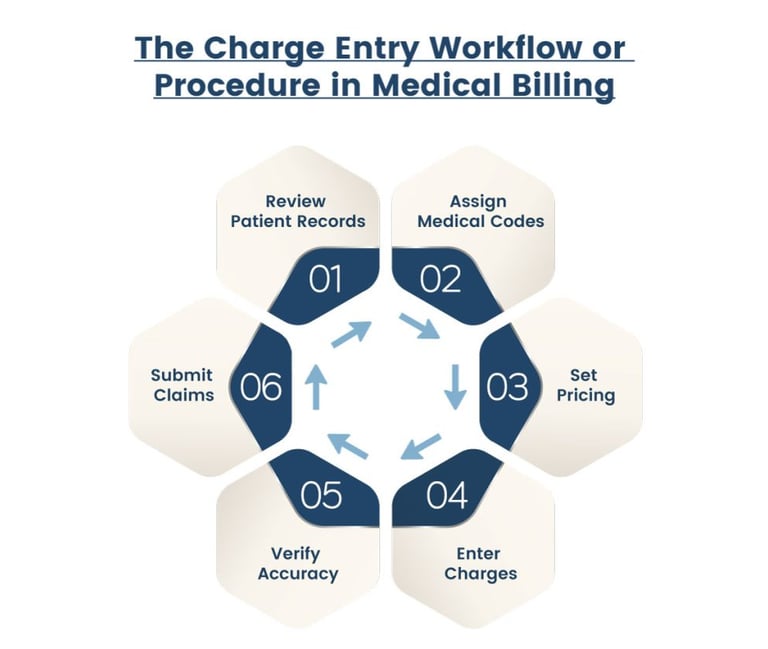
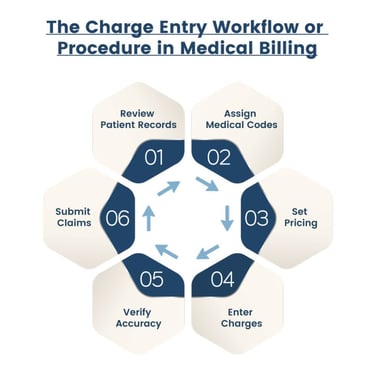
Charge Entry in Medical Billing
Charge entry in medical billing is the process of translating healthcare services into billable charges by assigning correct codes, ensuring accuracy, and submitting claims for reimbursement.
Charge entry is a crucial step in the medical billing process where healthcare services provided to a patient are translated into billable charges. This step ensures that all procedures, treatments, and services are accurately recorded and assigned the correct medical codes (CPT, HCPCS, ICD-10)
Charge Entry Process
Patient Information Verification
Provider and Service Details Entry
Procedure and Diagnosis Code Assignment
Charge Calculation
Modifiers Application
Claim Scrubbing & Validation
Charge Submission.
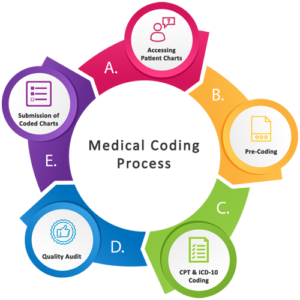
Medical Coding
Medical coding is a critical component of the medical billing process. It ensures that healthcare services are accurately documented, billed, and reimbursed.
Medical coding is vital for accurate billing, proper reimbursement, and efficient healthcare operations.
Ensures Accurate Billing & Payment – Prevents errors, reduces claim denials, and ensures providers get paid correctly.
Prevents Fraud & Compliance Issues – Helps avoid fraudulent claims and ensures compliance with regulations.
Standardization & Efficiency – Creates a universal language for billing, reducing administrative errors.
Supports Healthcare Data & Research – Helps track disease trends and improve medical research.
Enhances Patient Care – Maintains detailed, organized medical records for better treatment.
Medical coding ensures financial stability, compliance, and high-quality patient care in healthcare.


Pre-Authorization/Referrals
Pre-authorization and referrals enhance compliance, financial stability, and patient satisfaction.
Pre-authorization and referrals are essential components of medical billing that help ensure compliance, reduce financial risks, and improve the overall efficiency of healthcare services. Proper verification and authorization procedures can lead to better patient care and a more financially stable healthcare system.
Pre-authorization and referrals are crucial for ensuring smooth claim processing, minimizing
denials, and optimizing patient care.
Insurance Compliance – Required for certain procedures; failure leads to claim denials.
Prevents Claim Denials – Ensures insurance reimbursement and reduces appeals.
Cost Control – Prevents unnecessary procedures, lowering healthcare costs.
Faster Payments – Streamlines revenue cycle and improves cash flow.
Better Patient Experience – Reduces unexpected costs and delays.
Regulatory Compliance – Avoids penalties and contract violations.
Efficient Resource Use – Ensures coverage before service delivery.
Prevents Retroactive Denials – Avoids financial losses for providers.


Payment/EOB Posting
Payment/EOB posting ensures accurate billing, timely reimbursements, and effective claims management for improved cash flow and compliance.
Payment/EOB posting is crucial in medical billing for the following reasons:
Accurate Financial Records: Ensures payments are correctly recorded for proper reimbursement.
Claims Reconciliation: Helps match insurance payments with submitted claims, identifying discrepancies or denials.
Denial Management: Quickly flags denied or underpaid claims for resolution.
Compliance: Ensures adherence to payer requirements, reducing audit risks.
Cash Flow: Enables timely follow-ups on underpayments, improving cash flow.
Financial Reporting: Provides clear insights into revenue and forecasting.
Patient Experience: Reduces billing errors and improves patient satisfaction.
In essence, payment posting ensures accurate financial tracking, timely reimbursements, and smooth operations in medical billing.

Accounts Receivable
Accounts Receivable in medical billing ensures timely payments, improves cash flow, and support financial stability by tracking patient and insurance payments.
Accounts Receivable (AR) in medical billing is essential for ensuring timely payment for services rendered, supporting cash flow, and maintaining financial health. It tracks payments from insurance companies and patients, helping identify issues with claims or delayed payments. Efficient AR
management improves revenue cycle performance, reduces administrative costs, and provides valuable data for performance metrics. It also ensures compliance with regulations and enhances the patient experience by clearly communicating billing responsibilities. Ultimately, effective AR management helps healthcare organizations maintain a steady cash flow and avoid financial challenges.


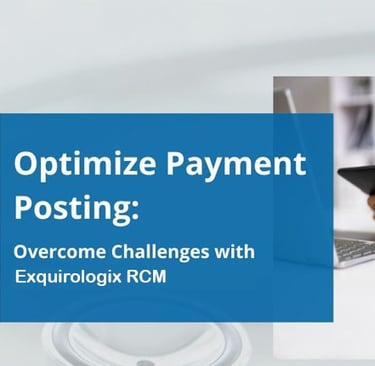
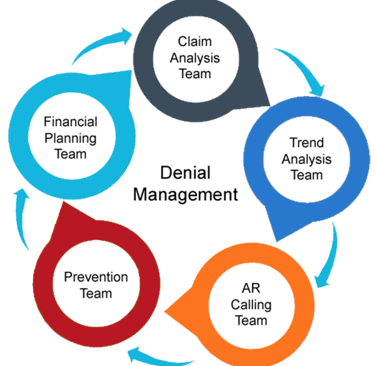
Denial Management
Denial management in medical billing ensures timely payments, improves cash flow, reduces errors, and optimizes reimbursements, enhancing financial stability for healthcare organizations.
Denial management is crucial in medical billing for several reasons:
Revenue Recovery: Helps recover payments from denied claims.
Cash Flow: Ensures timely payments and improves cash flow.
Trend Identification: Identifies recurring issues (e.g., coding errors).
Compliance: Keeps providers compliant with billing regulations.
Optimized Reimbursement: Increases reimbursement rates by addressing denial causes.
Patient Satisfaction: Resolves insurance issues, maintaining patient trust.
Cost Reduction: Lowers administrative costs by minimizing denials.
Resource Efficiency: Allows better allocation of staff and resources.
Overall, denial management ensures timely payments, improves efficiency, and supports
financial stability for healthcare organizations.
Appeals
Appeals in medical billing are vital for recovering denied claims, ensuring accuracy, and improving reimbursement processes.
Patient scheduling is crucial for medical billing as it ensures accurate coding and timely documentation, leading to correct billing. It helps in:
Appeals in medical billing are essential for recovering denied or underpaid claims. They help ensure accurate billing by correcting errors, clarify insurance coverage, and speed up
Reimbursement, improving cash flow. Appeals also strengthen relationships between providers and insurers, advocate for patients' rights, and prevent fraud. Ultimately, they help maintain financial stability for healthcare practices.


Solutions
Customized IT services for global business needs.
Support
Reach Us
© 2007. All rights reserved.
+91 779 500 9000
+91 080 2991 9024


